Skin Biopsy
INDICATIONS
Punch biopsy of inflammatory dermatoses can provide useful information when the differential diagnosis has been narrowed. Cutaneous neoplasms can be evaluated by punch biopsy, and the discovery of malignancy may alter the planned surgical excision procedure. Routine biopsy of skin rashes is not recommended because the commonly reported nonspecific pathology result rarely alters clinical management.
TECHNIQUE
- The area to be biopsied should be selected. Commonly selected sites are the most abnormal-appearing site within a lesion or the edge of an actively growing lesion. For suspected vasculitis a 4mm punch biopsy of a lesion edge with surrounding normal skin should be obtained. In general "young lesions" should be biopsied. Try to avoid biopsies below the knee.
- The skin is cleansed with povidone-iodine solution and anesthetized with1- 2 percent lidocaine with epinephrine. A 30-gauge needle is used to administer the anesthetic to limit discomfort.
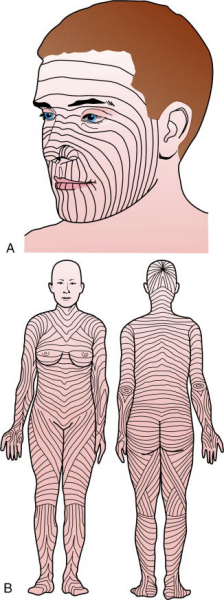
- The lines of least skin tension should be identified for the area to be biopsied. For example, on the arm, these lines run perpendicular to the long axis of the extremity. The incision line created by the suturing after the biopsy is performed will be oriented parallel to the lines of least skin tension. Physicians who cannot recall the line orientation for a specific body area should consult the widely published drawings of these lines.
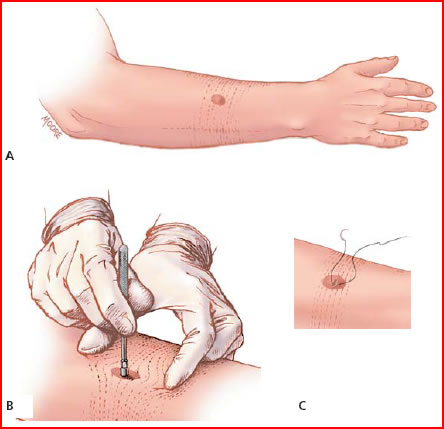
- The skin surrounding the biopsy site is stretched with the thumb and index finger of the non dominant hand (Figure below). The skin is stretched perpendicular to the lines of least skin tension. When the skin relaxes after the biopsy is performed, an elliptical-shaped wound remains that is oriented in the same direction as the lines of least skin tension (see Figure below for body/face skin tension lines). On the arm, the skin is stretched along the long axis of the extremity.
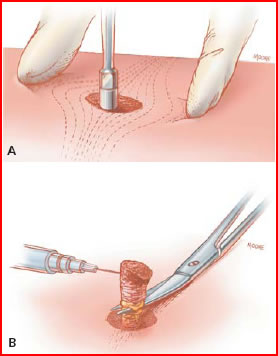
- The punch biopsy instrument is held vertically over the skin and rotated downward using a twirling motion created by the first two fingers on the dominant hand (Figure 2a). Once the instrument has penetrated the dermis into the subcutaneous fat, or once the instrument reaches the hub, it is removed.
- The cylindrical skin specimen is elevated with the anesthesia needle held in the non dominant hand. The use of forceps is discouraged because these instruments frequently cause crush artifact. Scissors held in the dominant hand cut the specimen free from the subcutaneous tissues (Figure 2b). The cut is made below the level of the dermis. The specimen should be placed in a formalin specimen bottle obtained from the lab, unless cultures are needed.
- The wound is closed, if necessary, with one or two interrupted nylon sutures: 5-0 nylon is used for most non facial areas, and 6-0 nylon for most facial areas. The suture generally creates good hemostasis, and antibiotic ointment and a bandage are then applied.
AmFamPhys VOLUME 65, NUMBER 6 / MARCH 15, 2002